The Day My Backbone Shattered—and the Surgeon Who Rebuilt It
A Backbone Surgical procedure Survivor’s Journey By way of Trauma, Belief, and the Science of Hope
You don’t take into consideration your backbone—till it’s the one factor you possibly can take into consideration.
That second got here for me within the wreckage of a automobile crash that shattered extra than simply bone. One minute, I used to be driving. The following, I used to be damaged—in and out. I had sustained an unstable lumbar fracture, the type of harm that modifications all the things. My backbone—the structural core of my physique—was compromised. I couldn’t sit up. I couldn’t stroll. I didn’t know if I ever would once more.
Enter Dr. Wylie Lopez, MD, an orthopedic backbone surgeon who focuses on moments like this. To him, this wasn’t simply surgical procedure. It was stabilization. Preservation. The chance to reclaim what had been violently taken from me.
And he did it—inside 24 hours.
Holding a Life in His Palms
Picture Credit score: Dr. Wylie Lopez
Once I requested Dr. Lopez what it feels prefer to actually maintain somebody’s potential to stroll—and even reside—in his fingers, he didn’t romanticize it.
“It’s some of the annoying elements of what I do,” he stated. “There’s numerous uncertainty in medication, particularly with trauma. Even a technically excellent job can have an unsure restoration. These are the conditions that maintain us up at evening.”
However that stress, he defined, is precisely why mastery issues.
“I give attention to the issues I can management—my approach, my decision-making, my fingers.”
These fingers saved my life.
Breaking the Myths Round Backbone Surgical procedure
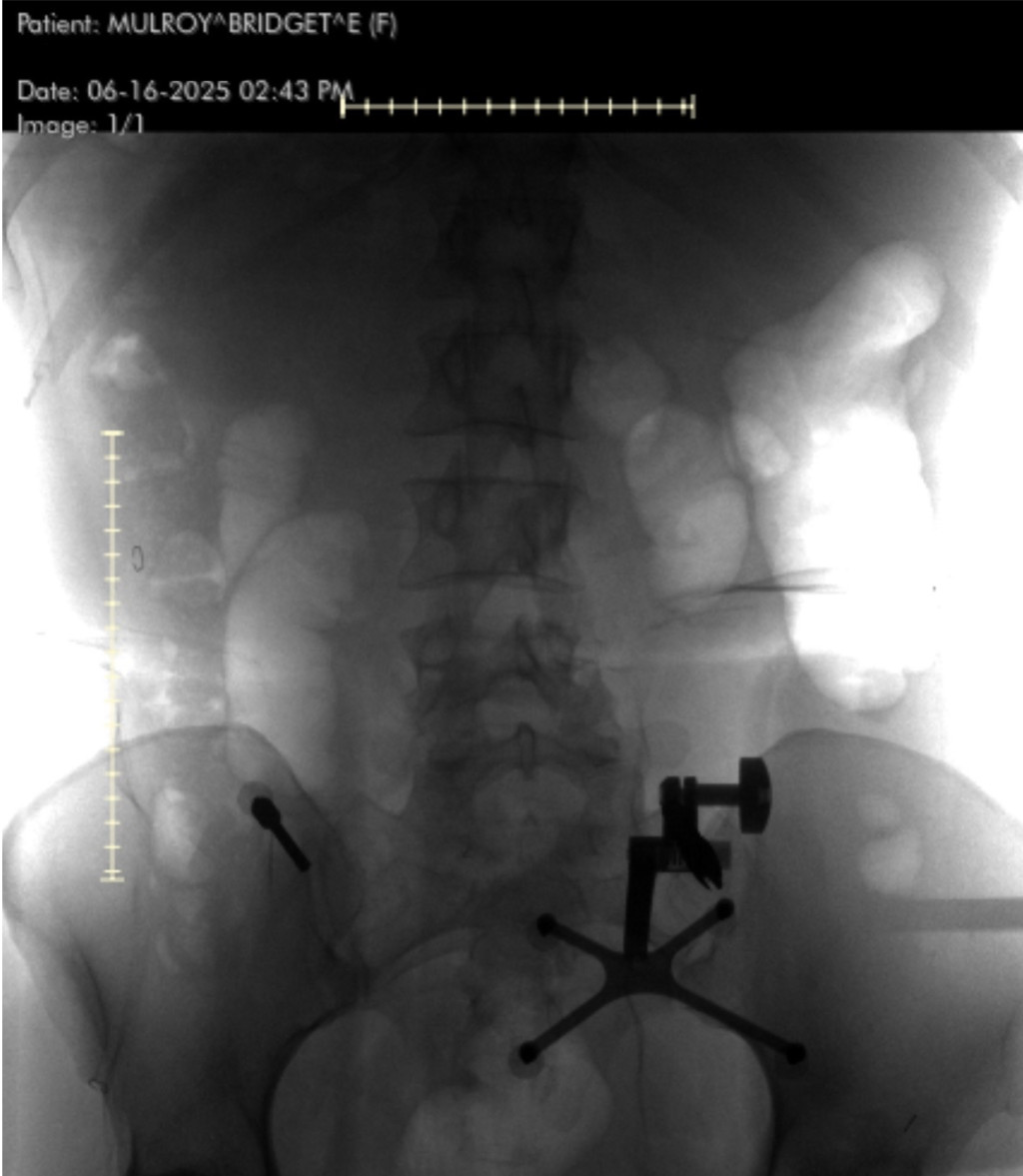
Picture Credit score: Bridget Mulroy
Earlier than my surgical procedure, I used to be terrified. I had heard all of the horror tales—paralysis, persistent ache, botched fusions, dependancy to ache meds. However Dr. Lopez sees these narratives as outdated and oversimplified.
“Backbone surgical procedure has reached a technological revolution,” he stated. “We now have robotics, augmented actuality, and minimally invasive methods that make even complicated surgical procedures safer and outcomes higher.”
One of many largest myths? That bodily remedy doesn’t work and that surgical procedure is inevitable.
“About 80% of my sufferers get higher with PT, train, weight reduction, and managing despair,” he defined. “I function on the opposite 20%. Surgical procedure is commonly the final line of protection.”
However in trauma circumstances like mine, that calculus modifications shortly.
The Science of Emergency Stabilization
“Once I realized your fracture was unstable,” Dr. Lopez informed me, “I knew you wouldn’t be capable to mobilize with out inner stabilization. Letting you attempt to stroll might’ve worsened the fracture, prompted spinal deformity, or led to nerve harm and persistent ache.”
As a substitute of utilizing an exterior brace, Dr. Lopez used {hardware}—screws and rods—to create inner assist.
“Technically, you didn’t have a spinal fusion,” he clarified. “You had spinal instrumentation and stabilization. A fusion requires bone grafts and biologic processes to encourage new bone progress.”
What he gave me, although, was simply as highly effective: a structurally sound backbone—and a second probability at mobility.
Contained in the Working Room
When Dr. Lopez described the precise process, I used to be floored by the precision concerned.
He carried out a minimally invasive posterior lumbar instrumentation from L2 to L5. Meaning he made small incisions guided by real-time navigation utilizing a machine known as the O-arm—a rotating intraoperative CT scanner. A localizing pin in my pelvis communicated with a pc, which informed him precisely the place to position every screw.
“As soon as the screws are inserted,” he defined, “I exploit an X-ray to position the rods. The important thing choices contain understanding which ranges to incorporate, guaranteeing screw trajectory is ideal, and having a plan if one thing doesn’t go proper.”
I requested: What occurs if one thing doesn’t go proper?
“If a screw is positioned too far ahead, it might hit main blood vessels. That might result in dying or extreme incapacity.”
He didn’t say this to scare me—he stated it as a result of that’s the extent of consequence backbone surgeons face each time they step into the OR.
Minimally Invasive, Maximally Transformative
So what does “minimally invasive” truly imply?
“It means lowering collateral harm,” Dr. Lopez stated. “We keep away from dissecting the massive muscle tissue of the backbone. Meaning much less blood loss, much less post-op ache, and sooner restoration. The identical applies to endoscopic and lateral-based approaches.”
Inside 24 hours of surgical procedure, I used to be standing. Strolling. Slowly, sure—however it felt miraculous.
“That’s as a result of the backbone was now not unstable,” he stated. “When you repair the issue mechanically, motion turns into tolerable once more. And the physique is extremely resilient.”
The Psychological Sport of Restoration
After all, restoration isn’t simply bodily—it’s emotional.
“The psychological half is half the battle,” Dr. Lopez informed me. “Folks with despair have worse outcomes, even with the identical surgical procedure. I encourage positivity and resilience as a result of it really impacts therapeutic.”
In my case, he stated my restoration was above common. Why?
“You’re younger, wholesome, and motivated. You even have a robust ache tolerance, which made bodily remedy extra manageable.”
He additionally emphasised how essential pre-injury health and psychological well being are in predicting outcomes.
“Most of my sufferers return to a traditional life, so long as they observe restrictions and handle danger elements like smoking or uncontrolled diabetes.”
Ache, Opioids, and the Steadiness of Belief
Ache administration is likely one of the most delicate elements of backbone surgical procedure restoration. The ache is actual—however so is the concern of opioid dependency.
“There must be a strong post-op ache plan,” he stated. “Clear boundaries, expectations, and generally a narcotics settlement. However we additionally go away room for compassion. If somebody is struggling, we work with them.”
A Future Constructed on Titanium—and Hope
Picture Credit score: Bridget Mulroy
I requested him what turns into of all of the {hardware}—the screws, rods, and implants—as soon as the backbone heals.
“They assist the physique by the therapeutic course of,” he stated. “As soon as bone progress stabilizes the section, it’s just like the {hardware} isn’t even there. But when a surgical procedure doesn’t heal correctly, the {hardware} can grow to be free, break, and even get contaminated.”
And what about these rumors of turning into a “human barometer”?
“We hear that loads,” he laughed. “There’s no definitive proof, however barometric stress could have an effect on tissues post-op. The jury’s nonetheless out.”
If You’re Afraid…
To anybody frozen by the concern of backbone surgical procedure—particularly these struggling in silence from persistent ache—Dr. Lopez had this to say:
“I strive to not push. My job is to teach. In the event that they ask what I’d do, I think about they’re my very own guardian and reply with that in thoughts.”
That’s what makes him particular. Not simply his surgical talent—however his humanity. He’s not simply chopping bone—he’s restoring lives.
My Life After Surgical procedure
At this time, I reside with out concern of collapse. With out the uninteresting, grinding ache that after outlined my each motion. I stroll. I journey. I reside. And I owe that to the science of contemporary spinal medication—and to Dr. Wylie Lopez, whose regular fingers held my future.
He says he remembers each affected person he’s handled with spinal wire harm and paralysis. He carries them with him.
I carry him with me, too—not simply within the screws and rods that stabilized my backbone, however within the religion I now have in my physique, my therapeutic, and what’s potential when medication meets miracle.
For those who’ve been informed your again is damaged—or that your ache has no resolution—know this:
There are folks like Dr. Lopez who dedicate their lives to rebuilding what feels shattered past restore.
There’s hope. There’s therapeutic.
And sure, there’s life on the opposite aspect of damaged.
Interview
1. Your fingers gave me again the flexibility to stroll. What does it really feel like, as a backbone surgeon, to fairly actually maintain somebody’s future mobility—and generally their life—in your fingers?
“It’s definitely some of the annoying elements of what I do. There may be numerous uncertainty in Medication and a part of my job is to grasp all of the issues which are in my direct management–issues I might be sure about, reminiscent of surgical approach and indicating the suitable surgical procedure for somebody. In sure cases, reminiscent of a extreme trauma with paralysis, even a technically excellent job can nonetheless be clouded by an unsure restoration. These are essentially the most annoying conditions and those that maintain us up at evening.”
2. What led you to specialise in backbone surgical procedure? Was there a defining second or private expertise that drew you to this discipline of drugs?
“It occurred very organically. In my coaching, I had the pleasure of working with some world-renowned surgeons. We spent many hours collectively working and seeing sufferers within the workplace. A normal curiosity in the subject material and the conclusion that I used to be turning into fairly good at it’s what led me to pursue extra time within the working room with these surgeons. As soon as I actually obtained to know these backbone surgeons, I noticed that I had loads in widespread with them and started pursuing extra alternatives to work with them. That led to extra circumstances, a stronger data base, and higher fingers. And thus, a backbone surgeon was born.”
3. Backbone surgical procedure carries an nearly legendary degree of concern for a lot of—pictures of paralysis, extended restoration, or everlasting incapacity. What are a few of the largest misconceptions you’ve encountered, and the way does trendy spinal medication problem these fears?
“Misconceptions definitely run wild on this discipline. Bodily remedy not working might be one of many largest ones. I discover that bodily remedy sometimes fixes about 80% of my sufferers and I find yourself working on the opposite 20%. It’s truly astounding how many individuals discover reduction simply from train, weight reduction, and optimization of co-morbidities and psychological well being (despair performs a giant function in restoration). One other huge one is folks simply assuming that they will do poorly after backbone surgical procedure as a result of everybody has a good friend with a horror story. In at this time’s world, backbone surgical procedure has reached a technological revolution marked by robotics, augmented actuality assisted, and minimally invasive surgical procedure which has reworked the sphere for the higher. These enabling applied sciences have made even essentially the most tough surgical procedures extra routine and have helped enhance affected person outcomes. That is higher for everybody concerned.”
4. You operated on me inside 24 hours after I used to be informed my backbone was damaged. From a scientific standpoint, what’s occurring within the physique when a spinal fracture like that happens—and why is well timed intervention so crucial?
“There’s a lot that goes on after the physique sustains a fracture. A very powerful from the attitude of a backbone surgeon is the way it finally impacts your mobility, backbone stability, and nerve integrity. If an individual lays in mattress motionless, they’ve a a lot larger danger of growing blood clots or pneumonia, which might be life threatening. That is why getting folks up and transferring is such an essential aim for surgeons. Once I realized that your fracture was unstable, I knew that you wouldn’t be capable to mobilize till your fracture was stabilized. If I allow you to stroll with an unstable backbone fracture, you would have developed worsening place of the fracture, a spinal deformity resulting in persistent ache and probably requiring a fair larger/extra morbid process, and even nerve harm from bony compression resulting in extremity deficits, incapacity, and persistent nerve ache.”
5. Many consider spinal surgical procedure ought to solely be used as a final resort. However it saved my life. In what eventualities is spinal fusion truly the most secure and only first-line therapy?
“There may be some nuance right here with the terminology. You underwent a spinal instrumentation and stabilization and not using a fusion. I used {hardware} to basically “brace” your backbone from the within (versus an exterior brace which might not have labored on this case). A spinal fusion requires biologic help from the physique along with stabilization of the section. That might imply utilizing bone graft and carpentry work to the bone that might facilitate signaling pathways that calls bone cells to the world to kind extra bone. Spinal fusions are sometimes required in cases the place we’re eradicating bone and know that we’re going to de-stabilize a section within the course of, after we are trying to vary the form of the backbone and need it to heal in that new place, or when there’s a extreme pathology that wants new bone to kind to totally stabilize the section in the long run.”
6. Are you able to stroll us by the steps of a posterior lumbar spinal instrumentation, just like the one I had—from incision to closure? What sorts of real-time choices do you must make within the OR when sudden complexities come up?
“The method behind a posterior instrumentation with stabilization is as follows (I did this minimally invasive so it’s barely completely different): I positioned a metallic localizing pin into your pelvis which talks to the pc within the room which helps us with actual time screw navigation. We spin a big machine known as an O-arm which performs in intraoperative CT scan which supplies us numerous details about your bones. We use that as an actual time navigation for putting the screws into the bones. We then used a particular marker to know precisely the place to position your incisions based mostly on the real-time suggestions from the navigation (we will maintain the a number of incisions small due to this expertise). As soon as the incisions are made, we dissect down the pores and skin, fascia, muscle, and all the way down to the bones of the backbone. From there I exploit the real-time navigation to know the trajectory of the screw and place each with a set of devices—first an axe to make a small gap within the bone, then a faucet to widen that gap a bit with a purpose to higher facilitate screw insertion, then the precise screws. As soon as the screws are inserted, I exploit an x-ray machine to assist me place the rods. The true choice making right here consists of the pre-operative planning and understanding which ranges to incorporate, the correct screw trajectory and to know if the suggestions from the reside navigation is correct, and what to do if a screw isn’t excellent.”
7. From a surgical perspective, what makes a multilevel spinal surgical procedure (like mine from L2 to L5) particularly complicated or high-stakes?
“It’s good to guarantee that the screws are positioned correctly or they might pull out or the fracture received’t heal. If the screws are by accident positioned a bit too anteriorly (which means too far ahead), they will cross the entrance of the backbone and hit one of many massive blood vessels; this might result in dying or extreme incapacity.”
8. We frequently hear the time period “minimally invasive” in spinal care, however what does that really imply in follow? How have surgical methods advanced over the previous decade to scale back trauma and enhance restoration?
“”Minimally Invasive” or MIS, is a time period used to explain a deviation from standard backbone surgical procedure that seeks to attenuate collateral harm to different constructions and enhance restoration. With MIS surgical procedure, there’s much less dissection of the large muscle tissue of the backbone which implies much less harm to these muscle tissue and a sooner return to operate, which for the physique is likely one of the most essential issues. The identical might be stated about different close by constructions with different kinds of MIS surgical procedure reminiscent of lateral-based oblique decompressions, tubular and endoscopic surgical procedures, and so forth.”
9. The trauma of a spinal harm isn’t simply bodily—it’s emotional. How do you think about the psychological and emotional toll of surgical procedure when working with sufferers? Do you see psychological resilience as a part of the therapeutic course of?
“The psychological a part of this course of is half the battle. I attempt to encourage sufferers to suppose positively and be resilient as it may contribute to their post-operative restoration (or lack thereof). Sufferers who’re extra motivated are inclined to work more durable with post-op mobility and bodily remedy and people with despair are proven to have [the] worst outcomes, even when the surgical procedure is similar.”
10. For individuals who concern shedding their independence after surgical procedure, what are you able to share about trendy restoration timelines and mobility outcomes? Is the thought of being “bedridden for months” outdated?
“Restoration is commonly extremely depending on the magnitude of the harm. We discover that the affected person’s pre-injury neurologic operate and bodily exercise standing performs a significant function of their post-operative restoration. Being bedridden for a backbone harm that doesn’t have any neurological modifications pre-operatively is kind of uncommon these days. After all, when you have a spinal wire harm then that image can drastically change.”
11. Put up-operative ache might be intense, however so is the concern of dependency on ache medicine. How do you assist sufferers stroll the road between managing ache successfully and avoiding long-term reliance on opioids?
“There needs to be post-operative ache plan that each affected person and doctor can agree on. Numerous physicians require a narcotics contract beforehand in order that there is no such thing as a confusion as to what the plan is. After all, everybody’s ache is completely different and there’s at all times wiggle room when a affected person is struggling. I feel setting clear boundaries goes a great distance with this a part of the patient-physician relationship.”
12. I used to be strolling inside 24 hours of main spinal surgical procedure. What does that say concerning the physique’s resilience—and the way a lot of that final result is made potential by surgical precision and planning?
“That half is solely depending on stabilization of the unstable fracture. As soon as that piece is now not displacing with easy actions (after fixing with screws and rods), standing, shifting, transferring, and so forth all turns into far much less painful. The physique should get used to the truth that it had surgical procedure and it has loads of resilience to beat that hurdle.”
13. How do you establish when a affected person really wants surgical procedure versus after they may profit extra from conservative therapy like bodily remedy, injections, or ache administration?
“It’s completely depending on their preliminary presentation. With fractures and spinal wire accidents, it’s usually based mostly on a algorithm that we observe—it begins with figuring out stability and understanding if the affected person has a neurologic harm or not. It’s truly MORE tough with the elective surgical procedures. It’s making an attempt to know the affected person’s state of affairs, how significantly better you suppose you may make them with an intervention, and the way a lot they’ve tried initially. In conditions the place sufferers are in ache however it’s manageable, I nearly at all times attempt to begin them off with 6 weeks of bodily remedy and a few kind of prescription energy ache medicine reminiscent of an anti-inflammatory. If that fails, relying on their MRI, we could strive injections or different types of therapy reminiscent of acupuncture, chiropractic care, muscle stimulation, therapeutic massage remedy, and so forth. I think about myself to be a conservative surgeon and surgical procedure is commonly the final line of protection.”
14. You’ve handled tons of, perhaps hundreds, of sufferers over time. Is there one case that stands out—one thing that modified the way you method your work or reminded you why you selected this occupation?
“I wouldn’t say there’s one explicit that stands out; there are lots of which have caught with me all through the years. Probably the most painful are younger sufferers who’ve sustained spinal wire accidents with paralysis. If you take name at a degree 1 trauma middle, you’ll meet these sufferers sooner or later in your profession. I bear in mind each one among them.”
15. Let’s discuss concerning the {hardware}—titanium rods, screws, cages. What function do they play long-term? Can sufferers really feel them indefinitely, or does the physique adapt?
“The entire level of the {hardware} is to help the physique in performing its pure course of. As soon as the fusion has matured, the physique will operate as if the {hardware} isn’t even there. In some cases, when a surgical procedure doesn’t heal correctly (pseudoarthrosis/nonunion), the {hardware} can loosen, break, or grow to be chronically contaminated. In these circumstances, they are often irritating and generally should be eliminated or changed.”
16. Some sufferers say they grow to be “human barometers” after backbone surgical procedure. Is there reality to climate sensitivity in relation to backbone well being, or is that extra anecdotal?
“It is a powerful one. There may be a lot anecdotal proof however there’s nothing that we will level to that definitively explains why it occurs. There may be some free proof that factors to variations within the temperature and barometric stress (atmospheric stress) affecting post-surgical tissue in a different way. The fact is, we don’t know.”
17. Backbone surgical procedure at this time is drastically completely different than it was 20 years in the past. What breakthroughs—whether or not in robotics, imaging, or approach—have most revolutionized the sphere?
“I feel the largest sport changers are robotics and endoscopic methods. Robotic assisted surgical procedure has leveled the taking part in discipline and has made the harder methods simpler to do. Endoscopic surgical procedure is a brand new type of extremely minimally invasive surgical procedure that enables sooner restoration instances and faster return to work with little to no narcotic use after surgical procedure. Not all sufferers are candidates for this kind of surgical procedure. It is a approach that I’m at present pursuing.”
18. There’s this concern that spinal surgical procedure limits an individual’s life eternally. However you had me strolling inside days. What sorts of lives do your sufferers sometimes return to—athletes, dad and mom, vacationers? Is a full life after surgical procedure nonetheless potential?
“There are completely different ranges to backbone surgical procedure. Greater surgical procedures can result in larger modifications in an individual’s life. Additionally it is very a lot depending on a affected person’s pre-injury/pre-surgery useful degree, dietary standing, age, and motivation. We all know that comorbidities reminiscent of uncontrolled diabetes, weight problems, and smoking can actually complicate somebody’s post-operative restoration and enhance the danger of a complication. I might say that the majority sufferers return to a traditional life so long as they observe the post-operative restrictions and reduce modifiable danger elements.”
19. At my follow-up, you informed me I used to be progressing sooner than common. In your expertise, what contributes to a super restoration? How a lot of that’s bodily, and the way a lot is psychological?
“You’re a younger/wholesome particular person with no medical issues and outlook on life. Folks such as you sometimes do nice! The most important query mark for a surgical procedure like yours is how individuals are going to tolerate post-operative ache. In your case, I might say you’ve got a robust ache tolerance which made your post-operative bodily remedy simpler to tolerate.”
20. For those who had been sitting throughout from somebody fearful of backbone surgical procedure—somebody in persistent ache however frozen by concern—what would you say to them, physician to human being?
“That is what I do each single day, and it’s extremely depending on their pathology and state of affairs. I attempt to by no means drive them in a selected course except it’s a dire circumstance. As a substitute, I consider that my job is to teach them about their choices and in the event that they ask me what I might do, I image them as one among my dad and mom earlier than giving them a solution.”